የሱፕራፓቴላር አቀራረብ በከፊል በተራዘመ የጉልበት አቀማመጥ ላይ ለሚገኝ የቲቢያ ኢንትራሜዱላሪ ጥፍር የተሻሻለ የቀዶ ጥገና አቀራረብ ነው። በሃሉክስ ቫልጉስ አቀማመጥ ላይ የቲቢያ ኢንትራሜዱላሪ ጥፍርን በሱፕራፓቴላር አቀራረብ ማከናወን ብዙ ጥቅሞች አሉት፣ ነገር ግን ጉዳቶችም አሉት። አንዳንድ የቀዶ ጥገና ሐኪሞች የቲቢያ 1/3ኛውን የቲቢያን ተጨማሪ-articular ስብራት በስተቀር ሁሉንም የቲቢያ ስብራት ለማከም SPN መጠቀምን የለመዱ ናቸው።
የ SPN አመላካቾች የሚከተሉት ናቸው
1. የቲቢያ ግንድ የተቆራረጠ ወይም የተከፋፈለ ስብራት። 2፤
2. የሩቅ ቲቢያል ሜታፊዚስ ስብራት፤
3. የዳሌ ወይም የጉልበት ስብራት ቀደም ሲል የነበረ የመተጣጠፍ ገደብ (ለምሳሌ፣ የዳሌ መገጣጠሚያ መበላሸት ወይም ውህደት፣ የጉልበት ኦስቲኦኮሮርስሲስ) ወይም የጉልበት ወይም የዳሌ መገጣጠሚያ ማጠፍ አለመቻል (ለምሳሌ፣ የዳሌው የኋላ መገጣጠሚያ መገጣጠሚያ መገጣጠሚያ መገጣጠሚያ፣ የፊንጢጣ አጥንት ስብራት)፤
4. የቲቢያ ስብራት ከቆዳ ጉዳት ጋር በኢንፍራፓቴላር ጅማት ላይ፤
5. ከመጠን በላይ ረጅም ቲቢያ ባለበት ታካሚ ላይ የቲቢያ ስብራት (የቲቢያው ቅርብ ጫፍ ብዙውን ጊዜ በፍሎሮስኮፒ ስር ለማየት አስቸጋሪ ነው የቲቢያ ርዝመት ፍሎሮስኮፒ ሊያልፍበት ከሚችለው ትራይፖድ ርዝመት በላይ ሲያልፍ)።
የመካከለኛ ቲቢያል ዲያፊዚስ እና የሩቅ ቲቢያል ስብራትን ለማከም ከፊል-የተራዘመ የጉልበት አቀማመጥ የቲቢያል ኢንትራሜዱላሪ የጥፍር ቴክኒክ ጥቅም የሚገኘው በመልሶ አቀማመጥ ቀላልነት እና በፍሎሮስኮፒ ቀላልነት ላይ ነው። ይህ አካሄድ የቲቢያን ሙሉ ርዝመት በጥሩ ሁኔታ ለመደገፍ እና የስብራቱን ቀላል የሳጊታል ቅነሳ ያለ ማዛባት (ምስል 1፣ 2) ያስችላል። ይህም በ intramedullary የጥፍር ቴክኒክ ለመርዳት የሰለጠነ ረዳት አስፈላጊነትን ያስወግዳል።
ምስል 1፡ ለኢንፍራፓቴላር አቀራረብ የኢንፍራሜዱላሪ የጥፍር ቴክኒክ የተለመደ አቀማመጥ፡ ጉልበቱ በፍሎሮስኮፒክ ዘልቆ የሚገባ ትራይፖድ ላይ በተጣበቀ ቦታ ላይ ነው። ሆኖም፣ ይህ አቀማመጥ የስብራት ብሎክን ደካማ አሰላለፍ ሊያባብሰው እና ስብራትን ለመቀነስ ተጨማሪ የመቀነስ ቴክኒኮችን ይፈልጋል።
ምስል 2፡ በአንጻሩ፣ በአረፋ መወጣጫ ላይ የተዘረጋው የጉልበት አቀማመጥ የስብራት ብሎክ አሰላለፍን እና ቀጣይ ማዛባትን ያመቻቻል።
የቀዶ ጥገና ቴክኒኮች
ጠረጴዛ/አቀማመጥ፡- ታካሚው በፍሎሮስኮፒክ አልጋ ላይ ተኝቶ ተኝቷል። የታችኛውን የእግሮች መጎተት ሊከናወን ይችላል፣ ነገር ግን አስፈላጊ አይደለም። የደም ቧንቧ ጠረጴዛው ለሱፕራፓቴላር አቀራረብ የቲቢያን ኢንትራሜዱላሪ ጥፍር በጣም ተስማሚ ነው፣ ነገር ግን አስፈላጊ አይደለም። ሆኖም፣ አብዛኛዎቹ የስብራት ማስተካከያ አልጋዎች ወይም ፍሎሮስኮፒክ አልጋዎች ለሱፕራፓቴላር አቀራረብ የቲቢያን ኢንትራሜዱላሪ ጥፍር ተስማሚ ስላልሆኑ አይመከሩም።
የአይፕሲላተር ጭኑን መሸፈን የታችኛውን ክፍል በውጫዊ ሁኔታ እንዲሽከረከር ይረዳል። ከዚያም የተጎዳውን እጅና እግር ከተቃራኒው ጎን በላይ ከፍ ለማድረግ የጸዳ የአረፋ መወጣጫ ጥቅም ላይ ይውላል፣ እና የተጣመመ የዳሌ እና የጉልበት አቀማመጥ የፒን እና የውስጥ ሜዱላሪ የጥፍር አቀማመጥን ለመምራት ይረዳል። ጥሩው የጉልበት መወዛወዝ አንግል አሁንም ክርክር እየተደረገበት ነው፣ ቤልትራን እና ሌሎችም 10° የጉልበት መወዛወዝ እና ኩቢያክ 30° የጉልበት መወዛወዝ እንደሚጠቁሙ ይጠቁማሉ። አብዛኛዎቹ ምሁራን በእነዚህ ክልሎች ውስጥ ያሉ የጉልበት መወዛወዝ አንግል ተቀባይነት እንዳለው ይስማማሉ።
ይሁን እንጂ፣ ኢስትማን እና ሌሎችም የጉልበት መወዛወዝ አንግል ቀስ በቀስ ከ10° ወደ 50° ሲጨምር፣ የፌሞራል ጣላ በመሳሪያው ፐርኮቴሪያን ዘልቆ መግባት ላይ የሚያሳድረው ተጽዕኖ ቀንሷል። ስለዚህ፣ የበለጠ የጉልበት መወዛወዝ አንግል ትክክለኛውን የውስጥ ሜዱላሪ የጥፍር መግቢያ ቦታ ለመምረጥ እና በሳጊታል ፕላን ውስጥ ያሉትን አንግል ጉድለቶች ለማስተካከል ይረዳል።
ፍሎሮስኮፒ
የC-ክንድ ማሽን ከተጎዳው እጅና እግር በጠረጴዛው ተቃራኒ በኩል መቀመጥ አለበት፣ እና የቀዶ ጥገና ሐኪሙ በተጎዳው ጉልበት ጎን ላይ ቆሞ ከሆነ፣ መቆጣጠሪያው በC-ክንድ ማሽን ራስጌ እና በአቅራቢያ መሆን አለበት። ይህም የቀዶ ጥገና ሐኪሙ እና የራዲዮሎጂ ባለሙያው መቆጣጠሪያውን በቀላሉ እንዲመለከቱ ያስችላቸዋል፣ የርቀት መጋጠሚያ ሚስማር ሲገባ በስተቀር። ምንም እንኳን ግዴታ ባይሆንም፣ ደራሲዎቹ የC-ክንድ ወደ አንድ ጎን እንዲዘዋወሩ እና የቀዶ ጥገና ሐኪሙ ደግሞ የሽምግልና መቆለፊያ ዊንጣ ሲነዳ ወደ ተቃራኒው ጎን እንዲዘዋወሩ ይመክራሉ። በአማራጭ፣ የቀዶ ጥገና ሐኪሙ ሂደቱን በተቃራኒው በኩል ሲያከናውን የC-ክንድ ማሽን በተጎዳው ጎን ላይ መቀመጥ አለበት (ምስል 3)። ይህ ደራሲዎቹ በብዛት የሚጠቀሙበት ዘዴ ነው ምክንያቱም የቀዶ ጥገና ሐኪሙ የዲስታል መቆለፊያ ጥፍሩን ሲያሽከረክር ከሜዲያል ጎን ወደ ጎን እንዲሸጋገር ስለሚያስገድድ።
ምስል 3፡ የቀዶ ጥገና ሐኪሙ በተጎዳው ቲቢያ ተቃራኒ በኩል ይቆማል፤ ይህም የሽምግልናው መጋጠሚያ ዊንጣ በቀላሉ እንዲነዳ ያስችለዋል። ማሳያው ከቀዶ ጥገና ሐኪሙ ፊት ለፊት፣ በሲ-ክንድ ራስ ላይ ይገኛል።
ሁሉም የአንቴሮፖስቴሪየር እና የመካከለኛ-ጎን ፍሎሮስኮፒክ እይታዎች የተጎዳውን እጅና እግር ሳያንቀሳቅሱ ይገኛሉ። ይህ ስብራቱ ሙሉ በሙሉ ከመስተካከሉ በፊት እንደገና የተጀመረውን የስብራት ቦታ ከመፈናቀል ይከላከላል። በተጨማሪም፣ የቲቢያ ሙሉ ርዝመት ያላቸው ምስሎች ከላይ በተገለጸው ዘዴ C-arnን ሳያዘንቡ ማግኘት ይቻላል።
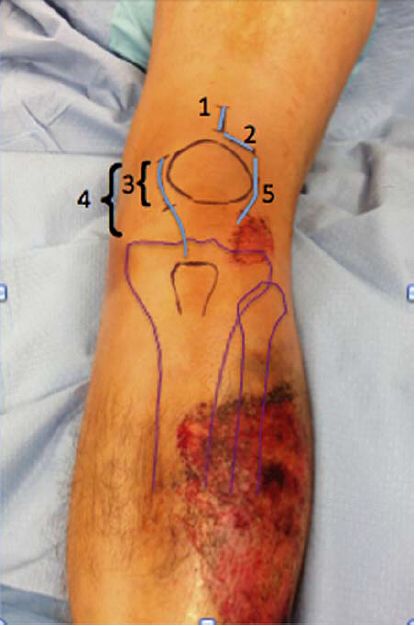
የቆዳ መቆረጥ ሁለቱም ውስን እና በአግባቡ የተራዘሙ መቆረጥዎች ተስማሚ ናቸው። ለኢንትራሜዱላሪ ጥፍር የፐርኩቴላር ሱፕራፓቴላር አቀራረብ የተመሰረተው ጥፍሩን ለማንቀሳቀስ በ3-ሴ.ሜ መቆረጥ ላይ ነው። አብዛኛዎቹ እነዚህ የቀዶ ጥገና መቆረጥ ቁመታዊ ናቸው፣ ነገር ግን በዶ/ር ሞራንዲ እንደተመከረው ተሻጋሪ ሊሆኑ ይችላሉ፣ እና ዶ/ር ቶርኔታ እና ሌሎች የሚጠቀሙበት የተራዘመ መቆረጥ በተጣመረ የፓቴላር ሱብሉክስሽን ባለባቸው ታካሚዎች ላይ ይታያል፣ እነዚህም በዋናነት መካከለኛ ወይም የጎን ፓራፓቴላር አቀራረብ አላቸው። ምስል 4 የተለያዩ መቆረጥዎችን ያሳያል።
ምስል 4፡ የተለያዩ የቀዶ ጥገና ቀዶ ጥገና አቀራረቦች ምሳሌ።1- ሱፕራፓቴላር ትራንስፓቴላር ጅማት አቀራረብ፤ 2- ፓራፓቴላር ጅማት አቀራረብ፤ 3- መካከለኛ የተወሰነ ቀዶ ጥገና ፓራፓቴላር ጅማት አቀራረብ፤ 4- መካከለኛ ረጅም ቀዶ ጥገና ፓራፓቴላር ጅማት አቀራረብ፤ 5- የጎን ፓራፓቴላር ጅማት አቀራረብ። የፓራፓቴላር ጅማት አቀራረብ ጥልቅ መጋለጥ በመገጣጠሚያ በኩል ወይም ከመገጣጠሚያ ቡርሳ ውጭ ሊሆን ይችላል።
ጥልቅ መጋለጥ
የፐርካኔቲየስ ሱፕራፓቴላር አቀራረብ በዋናነት የሚከናወነው ክፍተቱ እንደ ኢንትራሜዱላሪ ጥፍሮች ያሉ መሳሪያዎችን መተላለፊያ እስኪያገኝ ድረስ የኳድሪሴፕስ ጅማትን በረጅም ርቀት በመለየት ነው። ከኳድሪሴፕስ ጡንቻ አጠገብ የሚያልፈው የፓራፓቴላር ጅማት አቀራረብ ለቲቢያል ኢንትራሜዱላሪ የጥፍር ቴክኒክም ሊጠቁም ይችላል። ብልጭልጭ የሆነ የትሮካር መርፌ እና ካኑላ በጥንቃቄ በፓቴሎፌሞራል መገጣጠሚያ በኩል ያልፋሉ፣ ይህ አሰራር በዋናነት የቲቢያል ኢንትራሜዱላሪ ጥፍር የፊት-ከፍተኛ የመግቢያ ነጥብን በፌሞራል ትሮካር አማካኝነት ይመራል። ትሮካር በትክክል ከተቀመጠ በኋላ በጉልበቱ የጅማት ካርቱጅ ላይ ጉዳት እንዳይደርስ በቦታው መያያዝ አለበት።
ትልቅ የትራንስሊጋመንት ኢንሲጅን አቀራረብ ከሃይፐርኤክስቴንሽን ፓራፓቴላር የቆዳ መቆረጥ ጋር በማጣመር ጥቅም ላይ ሊውል ይችላል፣ በመካከለኛ ወይም በጎን አቀራረብ። ምንም እንኳን አንዳንድ የቀዶ ጥገና ሐኪሞች ቡርሳውን በቀዶ ጥገና ወቅት ሳይበላሹ ባያቆዩም፣ ኩቢያክ እና ሌሎችም ቡርሳዎቹ ሳይበላሹ መቆየት እንዳለባቸው እና ተጨማሪ የአካል ክፍሎች መዋቅሮች በበቂ ሁኔታ መጋለጥ እንዳለባቸው ያምናሉ። በንድፈ ሀሳብ፣ ይህ የጉልበት መገጣጠሚያን በጣም ጥሩ ጥበቃ ይሰጣል እና እንደ የጉልበት ኢንፌክሽን ያሉ ጉዳቶችን ይከላከላል።
ከላይ የተገለጸው አካሄድ የፓቴላውን ሄሚ-ዲስሎኬሽን ያካትታል፣ ይህም በመገጣጠሚያ ቦታዎች ላይ ያለውን የመገናኛ ግፊት በተወሰነ ደረጃ ይቀንሳል። በትንሽ የመገጣጠሚያ ክፍተት እና በጣም የተገደበ የጉልበት ማራዘሚያ መሳሪያ በመጠቀም የፓቴሎፌሞራል መገጣጠሚያ ግምገማ ማድረግ ሲከብድ፣ ደራሲዎቹ ፓቴላ በጅማት መለያየት በከፊል ሊፈርስ እንደሚችል ይመክራሉ። በሌላ በኩል መካከለኛው የሽግግር መቆረጥ በሚደገፉ ጅማቶች ላይ ጉዳት እንዳይደርስ ይከላከላል፣ ነገር ግን የተሳካ የጉልበት ጉዳት ጥገና ማድረግ ከባድ ነው።
የSPN መርፌ መግቢያ ነጥብ ከኢንፍራፓቴላር አቀራረብ ጋር ተመሳሳይ ነው። በመርፌ ማስገቢያ ወቅት የፊትና የጎን ፍሎሮስኮፒ የመርፌ ማስገቢያ ነጥብ ትክክል መሆኑን ያረጋግጣል። የቀዶ ጥገና ሐኪሙ መሪው መርፌ ወደ ፕሮክሲማል ቲቢያ በጣም ሩቅ እንዳይነዳ ማረጋገጥ አለበት። በጣም በጥልቀት ወደ ኋላ የሚነዳ ከሆነ፣ በፖስተርያል ኮሮናል ፍሎሮስኮፒ ስር በሚዘጋ ሚስማር እገዛ እንደገና መቀመጥ አለበት። በተጨማሪም፣ ኢስትማን እና ሌሎችም የመግቢያ ፒኑን በተዘረጋ የተወጠረ የጉልበት አቀማመጥ ውስጥ መቆፈር በቀጣይ በተዘረጋ ቦታ ላይ ስብራት እንደገና እንዲቀመጥ እንደሚረዳ ያምናሉ።
የመቀነስ መሳሪያዎች
ለመቀነስ ተግባራዊ መሳሪያዎች የተለያዩ መጠኖች ያላቸው የነጥብ ቅነሳ ፎርሴፕስ፣ የጭኑ አንሺዎች፣ የውጭ የማስተካከያ መሳሪያዎች እና ትናንሽ የስብራት ቁርጥራጮችን በአንድ ኮርቲካል ሳህን ለማስተካከል ውስጣዊ ማስተካከያዎችን ያካትታሉ። ከላይ ለተጠቀሰው የመቀነስ ሂደት የማገጃ ጥፍሮችም ጥቅም ላይ ሊውሉ ይችላሉ። የመቀነስ መዶሻዎች የሳጊታል አንግል እና የተሻጋሪ መፈናቀል ጉድለቶችን ለማስተካከል ያገለግላሉ።
የተተከሉ ተክሎች
ብዙ የአጥንት ውስጣዊ ማስተካከያ አምራቾች የቲቢያል ኢንትራሜዱላሪ ጥፍሮችን መደበኛ አቀማመጥ ለመምራት የመሳሪያ አጠቃቀም ስርዓቶችን አዘጋጅተዋል። የተዘረጋ የአቀማመጥ ክንድ፣ የሚመራ የፒን ርዝመት መለኪያ መሳሪያ እና የሜዱላሪ ማስፋፊያን ያካትታል። የትሮካር እና የብሌን ትሮካር ፒኖች የኢንትራሜዱላሪ የጥፍር መዳረሻን በጥሩ ሁኔታ መከላከላቸው በጣም አስፈላጊ ነው። የቀዶ ጥገና ሐኪሙ ከመንዳት መሳሪያው በጣም ቅርብ በመሆኑ የፓቴሎፌሞራል መገጣጠሚያ ወይም የፔሪያሪያል መዋቅሮች ላይ ጉዳት እንዳይደርስ የካኑላውን አቀማመጥ እንደገና ማረጋገጥ አለበት።
የመቆለፊያ ዊንጮች
የቀዶ ጥገና ሐኪሙ አጥጋቢ ቅነሳን ለማስቀጠል በቂ የመቆለፊያ ዊንጮችን ማስገባት አለበት። ትናንሽ የስብራት ቁርጥራጮችን (ቅርበት ወይም ሩቅ) ማስተካከል የሚከናወነው በአጠገብ ባሉት የስብራት ቁርጥራጮች መካከል ባለ 3 ወይም ከዚያ በላይ የመቆለፊያ ዊንጮችን በመጠቀም ወይም በቋሚ አንግል ዊንጮች ብቻ ነው። የቲቢያል ኢንትራሜዱላሪ የጥፍር ቴክኒክን በተመለከተ ያለው የሱፕራፓቴላር አቀራረብ ከዊንች መንዳት ቴክኒክ አንፃር ከኢንፍራፓቴላር አቀራረብ ጋር ተመሳሳይ ነው። የመቆለፊያ ዊንጮችን በፍሎሮስኮፒ ስር በትክክል ይንቀሳቀሳሉ።
የቁስል መዘጋት
በሚሰፋበት ጊዜ ተስማሚ የሆነ ውጫዊ ሽፋን ያለው መምጠጥ ነፃ የአጥንት ቁርጥራጮችን ያስወግዳል። ሁሉም ቁስሎች በደንብ መስኖ ያስፈልጋቸዋል፣ በተለይም የጉልበት ቀዶ ጥገና ቦታ። የኳድሪሴፕስ ጅማት ወይም የጅማት ሽፋን እና በተሰነጠቀበት ቦታ ላይ ያለው ስፌት ከዚያም ይዘጋሉ፣ ከዚያም የቆዳው እና የቆዳው መዘጋት ይከተላል።
የውስጠ-ሜዱላሪ ጥፍር ማስወገድ
በሱፕራፓቴላር አቀራረብ የሚነዳ የቲቢያል ኢንትራሜዱላሪ ጥፍር በተለየ የቀዶ ጥገና ዘዴ ሊወገድ ይችል እንደሆነ አሁንም አከራካሪ ነው። በጣም የተለመደው አካሄድ ኢንትራሜዱላር የጥፍር ማስወገጃ ትራንስአክቲካል ሱፕራፔቴላር አቀራረብ ነው። ይህ ዘዴ 5.5 ሚሜ ባዶ መሰርሰሪያ በመጠቀም በሱፕራፔቴላር ኢንትራሜዱላሪ የጥፍር ቻናል ውስጥ በመቆፈር ጥፍሩን ያጋልጣል። ከዚያም የጥፍር ማስወገጃ መሳሪያው በቻናሉ ውስጥ ይገፋል፣ ነገር ግን ይህ እንቅስቃሴ አስቸጋሪ ሊሆን ይችላል። የፓራፓቴላር እና የኢንፍራፔቴላር አቀራረቦች ኢንትራሜዱላር ጥፍሮችን ለማስወገድ አማራጭ ዘዴዎች ናቸው።
አደጋዎች የቲቢያል ኢንትራሜዱላሪ የጥፍር ቴክኒክን በተመለከተ የሱፕራፓቴላር አቀራረብ የቀዶ ጥገና አደጋዎች በፓቴላ እና በፌሞራል ታለስ ካርቱጅ ላይ የሚደርስ የሕክምና ጉዳት፣ በሌሎች የውስጥ-articular መዋቅሮች ላይ የሚደርስ የሕክምና ጉዳት፣ የመገጣጠሚያ ኢንፌክሽን እና የውስጥ-articular ፍርስራሾች ናቸው። ሆኖም ግን፣ ተዛማጅ ክሊኒካዊ የጉዳይ ሪፖርቶች እጥረት አለ። ቾንድሮማላሲያ ያለባቸው ታካሚዎች በሕክምና ምክንያት ለሚመጡ የ cartilage ጉዳቶች የበለጠ ተጋላጭ ይሆናሉ። በፓቴላር እና በፌሞራል አርቲካል ወለል መዋቅሮች ላይ የሚደርስ የሕክምና ጉዳት ይህንን የቀዶ ጥገና ዘዴ የሚጠቀሙ የቀዶ ጥገና ሐኪሞች በተለይም ትራንስአክቲቭ አቀራረብን የሚጠቀሙበት ዋና ጉዳይ ነው።
እስከዛሬ ድረስ፣ ከፊል-ኤክስቴንሽን ቲቢያል ኢንትራሜዱላሪ የጥፍር ቴክኒክ ጥቅሞች እና ጉዳቶች ላይ ምንም ስታትስቲካዊ ክሊኒካዊ ማስረጃ የለም።
የፖስታ ሰዓት፡- ጥቅምት-23-2023